This guide details the diagnostic approach to hypercalcaemia in dogs, covering clinical signs (anorexia, lethargy, PU/PD), causes and diagnostic steps. Key insights include interpreting CBC/biochemistry (albumin, globulins, ionised calcium), imaging (radiographs, ultrasound), and specific tests like PTH/PTH-rp.
The regulation of serum calcium is complex and involves the parathyroid glands, kidneys, intestine and bone. The main hormones involved in the regulation of calcium metabolism are parathyroid hormone (PTH) and 1,25 dihydroxyvitamin D3 (calcitriol).
The severity of clinical signs depend upon the magnitude of hypercalcaemia, duration and rate of onset.
- If tCa > 3.5 mmol/L (14 mg/dL) or iCa > 1.6 mmol/L (6.4 mg/dL): clinical signs are usually present.
- If tCa > 4.5 mmol/L (18 mg/dL), or iCa > 2.2 mmol/L (8.8 mg/dL): the patient is usually critically ill.
Clinical signs of hypercalcaemia in dogs
Clinical signs depend upon the magnitude of hypercalcaemia, duration and rate of onset, and they can be related to the hypercalcaemia itself and/or to the underlying disease causing hypercalcaemia.
Clinical signs may include:
- Common:
- anorexia
- lethargy
- dehydration
- weakness
- PU/PD
- vomiting
- azotaemia
- Less common:
- constipation
- twitching
- seizures
- cardiac arrhythmias
- hypertension
- urolithiasis
Aetiology of hypercalcaemia in dogs and diagnostic approach
The causes of hypercalcaemia can be remembered using the following mnemonic: HARDIONS-G
- H: Hyperparathyroidism
- A: Addison's disease
- R: Renal disease
- D: Hypervitaminosis D (cholecalciferol rodenticides, diet, plant intoxication, vitamin D skin preparations-treatment for psoriasis)
- I: Idiopathic (only cats)
- O: osteolytic bone lesions (e.g. osteomyelitis, hypertrophic osteodystrophy)
- N: neoplasia (lymphoma and anal sac adenocarcinoma are the most common but also others: multiple myeloma, carcinomas, thymoma)
- S: spurious (artefact, lipaemia, haemoconcentration)
- G: granulomatous disease:
- Fungal (most common: blastomycosis, histoplasmosis, cryptococcosis, coccidioidomycosis)
- Dermatitis
- Panniculitis
- Injection reaction
Figure 1 - Diagnostic approach to hypercalcaemia in dogs

The diagnostic approach to hypercalcaemia should start with a thorough history and clinical examination. Sometimes the cause of hypercalcaemia might be evident/suspected just on physical examination.
Check for potential neoplastic or granulomatous disease:
- Lymphadenomegaly
- Rectal palpation: anal sac mass might be suggestive of anal sac adenocarcinoma (sometimes these can be really small!)
- Hepato/splenomegaly
- Muffled heart/lung sounds suggestive of mediastinal mass, pleural effusion
- Pain on bone/spinal palpation: multiple myeloma, metastatic neoplasia, granulomatous disease, osteomyelitis
If any of the above is present, consider:
- Diagnostic imaging: radiographs/ultrasound/CT
- Fine needle aspirates
- Albumin:
- Hypoalbuminaemia + normal total calcium
- Artefactual: hypoalbuminaemia can result in lower total calcium levels and mask ionised hypercalcaemia or normal ionised calcium. Do not use adjustment formulas to correct the tCa as these formulas do not accurately predict iCa concentration.
- Hypoalbuminaemia + hypercalcaemia:
- Granulomatous, inflammatory, neoplastic disease (ionised)
- Renal disease (total)
- Addison's disease (total)
- Hypoalbuminaemia + normal total calcium
- Increased total proteins/total globulins:
- Consider performing serum protein electrophoresis:
- Monoclonal gammopathy: most likely neoplasia
- Polyclonal gammopathy: most likely granulomatous/infectious disease
- Consider performing serum protein electrophoresis:
- Ionised calcium (iCa):
- Handling the sample for ionised calcium measurement:
- Ideally, measure ionised calcium immediately after collection
- Do not use EDTA or citrate tubes (calcium chelator)
- Serum is preferred over lithium heparin tubes (ideally not serum-separator tubes or gel tubes as they can falsely increased ionised calcium)
- Avoid exposure to air or inclusion of air bubbles into the tube as this will decrease ionised calcium
- Do not freeze (falsely decreased ionised calcium due to alkalinization of the sample during frozen storage)
- Ionised calcium (serum/heparin sample) is stable after storage for 72 hours at 23 ̊ C or 4 ̊ C and for 7 days at 4 ̊ C.
- Use of serum collected anaerobically and stored at 4 ̊ C allows sufficient time for shipment to a reference laboratory
- Normal ionised calcium + increased total calcium: the most likely cause would be laboratory error, interference (handling sample, pH, storage conditions, etc) or chronic renal disease
- Handling the sample for ionised calcium measurement:
- Azotaemia:
- Azotaemia could suggest chronic renal disease, however hypercalcaemia also causes dehydration, reduced GFR, nephrocalcinosis and interstitial nephritis.
- Other tests might be necessary to support primary renal disease (UP/C, abdominal ultrasound to evaluate renal size, echotexture and architecture)
- Electrolytes: hyperkalaemia, hypochloraemia and hyponatraemia suggest hypoadrenocorticism; atypical hypoadrenocorticism should also be considered in the absence of electrolyte abnormalities if history and/or clinical findings are suggestive
- Hyperphosphataemia:
- CKD, hypervitaminosis D
- If tCa x P > 60-70 mg/dL (in SI units [mmol/L] >5) there is an increased risk of soft tissue mineralisation and nephrotoxicity. The higher risk is associated with CKD and hypervitaminosis D.
- Venous blood gases: metabolic acidosis worsens signs of hypercalcaemia (increases iCa)
- ACTH-stimulation test/basal cortisol: if suspicion of hypoadrenocorticism
- Diagnostic imaging:
- Thoracic radiographs/CT: mediastinal mass (lymphoma, thymoma, granulomatous disease), alveolar, interstitial or nodular pattern (neoplastic and granulomatous disease), microcardia (hypoadrenocorticism)
- Abdominal ultrasound/CT:
- Assessment of the kidney architecture will help determine if the azotaemia is cause or consequence of hypercalcaemia
- Adrenal glands
- Hepato/splenomegaly: neoplastic and granulomatous disease
- Urolithiasis
- Neck ultrasound: primary hyperparathyroidism
- Bone/spinal radiographs: osteomyelitis, granulomatous disease, multiple myeloma, lymphoma, metastatic disease
- PTH/PTH-rp in case all other causes have been ruled out or Keeshond
- Consider urine antigen tests: blastomycosis and histoplasmosis
- Consider blood antigen tests: cryptococcosis and coccidioidomycosis
|
Disease |
tCa |
iCa |
Biochemistry |
Electrolytes |
PTH |
PTHrp |
Vit D |
Imaging |
|
Primary hyperparathyroidism |
↑/N |
↑ |
N |
↓ |
↑ |
↓ |
|
|
|
Addison’s disease |
↑ |
Azotaemia/N |
↑K + ↓Na/N |
↓ |
|
|||
|
CKD |
↑/N |
Azotaemia/N |
N/↑ |
↓ |
|
|||
|
Hypervitaminosis D |
Azotaemia/N |
N |
|
|||||
|
Bone disease |
↑/N |
N |
N |
|
||||
|
Lymphoma |
↑/N |
↑ |
N |
N |
↓ |
↑ |
|
|
|
AGASACA |
↑/N |
↑ |
N |
N |
↓ |
↑ |
|
|
|
Multiple myeloma |
↑/N |
↑ |
↑GLOB |
N |
↓ |
N/↑ |
|
|
|
Granulomatous disease |
↑/N |
↑/N |
↑GLOB |
N |
↑ |
|
References
- Feldman EC, Nelson RW, Reusch CE, Scott-Moncrieff JCR, Behrend E: Canine and feline endocrinology. 4th ed. St. Louis: Elsevier, 2015
- Galvao JB, Schenck P, Chew D. A Quick Reference on Hypercalcemia. Vet Clin North Am Small Anim Pract. 2017 March; 47(2):241-248.
- Skelly B. Primary hyperparathyroidism. In: Textbook of Veterinary Internal Medicine. Eds Ettinger S, Feldman E & Coté E. 8th ed. St. Louis: Elsevier, 2017Schenck P, Chew D, Nagode L and Rosol T. Disorders of Calcium: Hypercalcemia and Hypocalcemia. In: Fluid, Electrolyte, and Acid-Base Disorders in Small Animal Practice || 2006.
Explore more

Jun 11, 2025 3:17:39 PM
Diagnosis and treatment of urinary incontinence in dogs
This article covers diagnosing and treating urinary incontinence in dogs, which involves...
Read more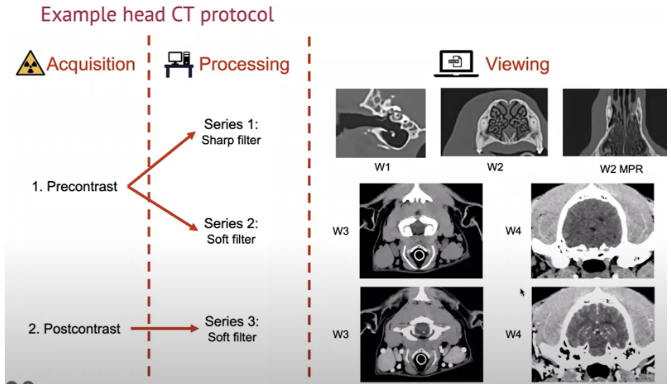
Jun 11, 2025 3:17:39 PM
How and When to Perform CT Reconstructions for Veterinary Patients
CT reconstructions are a vital tool in veterinary diagnostics, providing detailed images for...
Read more
%20(1).jpeg?width=75&height=75&name=Carolina%20Arenas%20(Default%20-%20Team%20Sheet)%20(1).jpeg)